Ophthalmologica Award lecturer reviews the challenges faced in demonstrating the efficacy of investigational treatments for atrophic retinal diseases and possible solutions
Geographic atrophy (GA) secondary to age-related macular degeneration (AMD), and Stargardt disease (STGD) are leading causes of blindness in the elderly and working-age populations, respectively. While no therapy for these diseases has yet been proven effective in terms of (pre-specified) visual function benefits, the recent commercialisation of two drugs for GA secondary to AMD, which were shown to improve imaging-based surrogate outcome measures, suggests this disease might be treatable.
In the Ophthalmologica Lecture, Maximilian Pfau, MD, Institute of Molecular and Clinical Ophthalmology, University Eye Hospital, Basel, Switzerland, will review how inter-patient variability in disease progression rates and the use of structural and functional endpoints that are unresponsive to treatment effects have challenged the ability to demonstrate the efficacy of investigational treatments for the two atrophic retinal diseases. Presenting work from his research group, Dr Pfau will provide a framework for overcoming the existing challenges.
Dr Pfau will explain that demonstrating the benefit of treatments for GA secondary to AMD and STGD requires enrolling fast-progressing patients in clinical trials and is further enabled by recruiting a homogenous cohort in which between-patient variability in progression rates is minimised. He will describe research identifying parameters for selecting a homogenous group of fast-progressing patients and how this information is being implemented in the design of ongoing clinical trials.
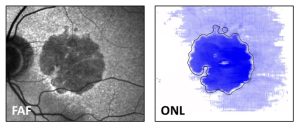
The figure shows a fundus autofluorescence image (FAF) and en-face projection of the outer nuclear layer (ONL) thickness of a patient with geographic atrophy secondary to age-related macular degeneration. Blue colours denote ONL thinning beyond normal variation. It is evident that photoreceptors are not only lost within the area of atrophy but also far beyond the main atrophic lesion.
In the second part of his lecture, Dr Pfau will explain that the structural endpoints employed in clinical trials, eg, measuring progression of retinal pigment epithelium (RPE) atrophy in fundus autofluorescence imaging or ellipsoid zone loss in optical coherence tomography imaging, reflect trailing disease boundaries (slowing of RPE atrophy progression) that hypothetically are partially unresponsive to treatment effects because their target is RPE cells that may be “beyond the point of no return”. He will present findings from research conducted by his group indicating that measurements focusing on the leading disease front, ie, photoreceptor preservation, are more optimal for revealing early therapeutic effects.
Finally, Dr Pfau will describe how to relate the earliest structural changes to visual dysfunction. In doing so, he will present the work his group has done developing microperimetry techniques, which include validation of a novel microperimetry device and the development of patient-tailored perimetry for GA secondary to AMD that allows for high-resolution testing able to monitor the progression of RPE atrophy with exceptional sensitivity.
Dr Pfau will also present the work by his group leading to the development of artificial intelligence models that infer retinal light sensitivity from OCT data. He will explain how these approaches are extremely helpful for contextualising imaging data from patients unsuitable for extensive functional testing and suggest that ‘inferred retinal light sensitivity’ could serve as a quasi-functional surrogate endpoint in future clinical trials.
Dr Pfau will deliver the Ophthalmologica Lecture at 13:00 on Saturday, 7 October 2023, in Elicium


