Delegates attending the session on non-neovascular age-related macular degeneration (AMD) on Saturday morning heard information that has important relevance for researchers and clinicians as treatments for geographic atrophy (GA) have become available and others are emerging.
The session began with Dr Christine Curcio (United States) reviewing new insights into the pathophysiology of geographic atrophy (GA) derived from combining histology with the cross-sectional view of optical coherence tomograph (OCT) that allows determination of how tissue layers beyond the retinal pigment epithelium (RPE) contribute to GA progression.
Dr Curcio showed that GA begins over individual drusen deposits as the external limiting membrane descends their sloping slides, the photoreceptors far from the choroid degenerate before the RPE, and Müller glia initiate and expand the atrophy.
“GA is a severe disease visible in vivo in cellular detail. Photoreceptor depletion, reactive gliosis, and adhesion add up to this severe disease,” she said.
“Many initiatives to treat GA predated this level of information about its severity. Based on this research, we should collectively think about intervening much earlier in the AMD progression, for example at the level of drusen.”
Speaking about imaging and artificial intelligence (AI)-based biomarkers in GA and precursor lesions, Dr Steffen Schmitz-Valckenberg (United States) noted that classification and differential diagnosis of GA remains key for research and patient management. In his talk he showed that high-resolution retinal imaging allows mapping of different precursor lesions and patterns leading to atrophy that may have an impact on the further disease course, including functional implications.
Dr Schmitz-Valckenberg concluded, “Image analysis based only on conventional qualitative assessment is not meaningful. This opens the door for use of AI-based algorithms as a promising tool to better understand the underlying mechanisms of atrophy development and progression, particularly in the era of new emerging therapies.”
Dr Maximilian Pfau (Switzerland) discussed the important topic of functional endpoints for evaluating outcomes in GA trials. He began with a discussion of the insufficiency of chart-based vision testing and then reviewed research identifying alternatives.
Dr Pfau concluded that clinical trials in AMD can be enhanced by spatially-specific testing (ie, patient-tailored microperimetry 1.0 and 2.0 workflow), photoreceptor-specific testing (fundus-controlled dark adaptometry), and inferred sensitivity mapping, which ideally should be used only in conjunction with functional evaluation
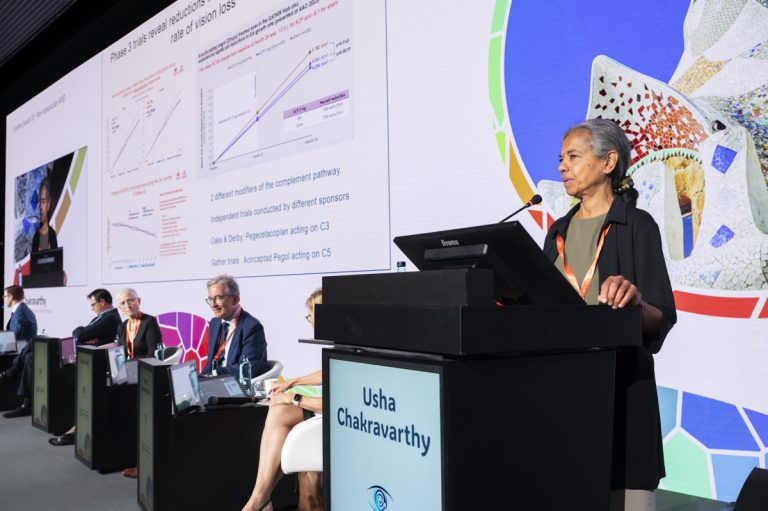
Dr Usha Chakravarthy (United Kingdom) addressed patient selection for complement inhibitor therapy. She reviewed the efficacy and safety results from the phase 3 clinical trials investigating pegcetacoplan and avacincaptad pegol and the occurrence of retinal vasculitis events in postmarketing experience that led the American Society of Retinal Specialists Research and Safety in Therapeutics Committee to development recommendations for patient selection and counseling.
Dr Chakravarthy also discussed findings from a recently published paper she coauthored in which a systematic examination of structure and function was undertaken to yield insights for selecting clinical trial endpoints and application to case selection in routine care.
Putting all of the information together, she concluded by presenting the following list of “optimal case selection attributes”: potential for rapid GA expansion; residual central visual function worth saving; juxta/extrafoveal GA location; fellow eye with visual loss due to GA (logMAR 1.0 or worse); and low risk for vasculitic complications identified by absence of any prior history of uveitis or diseases indicating systemic immune dysregulation.
Dr Philip Rosenfeld (United States) reported real world-experience using intravitreal pegcetacoplan for treating GA in patients seen at Bascom Palmer Eye Institute, Miami, FL. His presentation was based on data from 109 eyes followed for at least 6 months, including 84 eyes that had at least 12 months of follow-up and 56 that had prior annual visits.
As important take-home messages, Dr Rosenfeld said the research showed pegcetacoplan reduced the annualised growth rate of GA by about 41% in eyes with 1-year follow-up. In addition, it found that foveal and non-foveal GA had similar growth rates and similar responses to the therapy.
Noting that the treatment did not slow obvious VA loss, he also stated an important message for patient counseling.
“I say this over and over to my patients. This treatment is not going to improve vision. It is slowing disease progression.”
Registered attendees can watch the session On Demand.